New treatment for patients with rare liver cancer
At time of diagnosis, 45% of patients with neuro-endocrine tumors (NETs) present with metastasis. The overall 5-year survival rate of patients with NETs is approximately 60%. New advancements have been made in the treatment of NETs. IV administered somatostatin-bound radionuclides (i.e.lutetium-177-dotatate) have been shown to improve tumor response rates and survival. Despite of the increased tumor response rate and survival, liver metastasis still remain the major cause of morbidity and mortality in these patients.
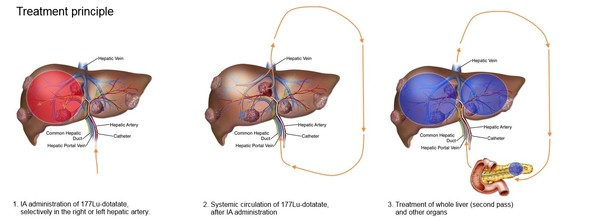
The so-called European Neuro-Endocrine Tumor Society Centers of Excellence of the Erasmus MC, UMC Utrecht and AVL-NKI join forces, in collaboration with the producer of lutetium-177-dotatate, to improve treatment for patients with liver metastases. We propose a phase I multi-center study in which patients with NETs with liver metastasis are treated via a catheter in the hepatic artery that feeds the tumors. With this method we aim to improve the radiation absorbed dose in the treated tumors. An increased tumor absorbed dose may lead to better outcome. At the end of this study we are able to say whether administration of the drug lutetium-177-dotatate straight in the tumor feeding artery leads to improved targeting and response.
Introduction: The aim was to investigate whether tumor uptake in liver metastases can be enhanced by intra-arterial (IA) administration of lutetium-177-dotatate (Lutathera®, AAA) via the hepatic artery, in order to improve tumor response without increasing toxicity.
Methods: In this prospective RCT, a total of 27 patients with grade 1-2 NET, and bi-lobar liver metastases were randomised to receive IA lutetium-177-dotatate in either the left or right hepatic artery for four consecutive cycles. The other liver lobe was treated via a 'second-pass' effect and was used as a control lobe. Up to 3 tumors per liver lobe were identified as target lesions at baseline (>3 cm). Tumor-to-normal (T/N) uptake ratios on 24h post-treatment SPECT/CT were calculated for each target lesion using the mean uptake and peak uptake (mean uptake in 1 cm diameter sphere around maximum uptake voxel), and compared between IA-treated lobe (IAL) and control lobe (CL) using paired-samples t-test. Furthermore, response was recorded according to RECIST 1.1 at 3 and 6 months post-treatment.
Results: A non-significant increase in both T/Nmean and T/Npeak uptake ratio was observed in the IAL: T/Nmean (SE): CL = 17.4 (3.9) vs. IAL = 19.1 (3.6) (p = 0.270); T/Npeak (SE): CL = 35.1 (7.8) vs. IAL = 41.3 (8.2) (p = 0.063). The average increase in T/Nmean = 1.76 (95% CI -1.45 – 4.98), T/Npeak = 6.2 (95% CI -0.35 – 12.8). Overall, 70% of patients showed an increase in T/Npeak ratio. Tumor response rates were identical (25% PR and 75% SD at 3 months; 36% PR, 59% SD and 5% PD at 6 months in both IAL and CL).
Conclusion: No significant increase in hepatic tumor uptake on SPECT/CT after 24h, and no difference in response at 3 or 6 months follow-up could be identified after intra-arterial administration of lutetium-177-dotatate.